The couples found with a male-factor infertility usually begin their evaluation with routine laboratory investigations. While this initial phase is very important, going through the same diagnostic step routinely may not always provide any new answers. Many men go through emotional fatigue and frustration, as changes in lifestyle or medications do not result in any changes in outcomes. At this point, this is where clinicians dig deeper for hidden causes beyond surface findings.
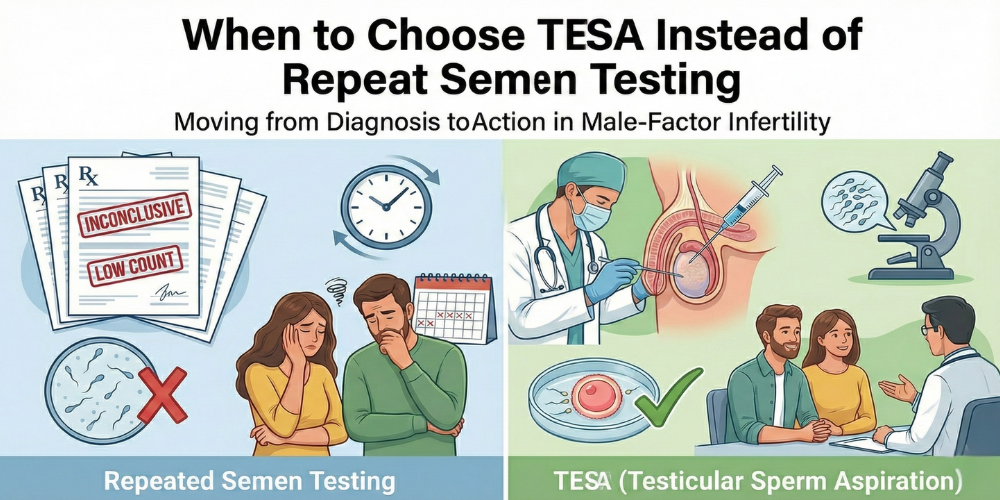
Basic semen analysis reflects what is present in ejaculate at the time and does not verify if sperm production is taking place inside the testes. Withheld explanation for why sperm are not being produced or why there is severe reduction of sperm in numbers The outcome of series of repeated tests indicates similar results; thus, keeping on testing for the same parameter is probably delaying the intervention we would have taken at that very time.
It is customary for doctors to recommend further testing if borderline results happen to be influenced by the temporary condition, like fever, stress, or recent illness. Usually, repeating these kinds of tests won't change anything once they are consistent in their results for several occasions. Instead, it delays certain treatments while adding to anxiety to couples already under stress.
A semen analysis test becomes less informative when it repetitively reaffirms a very low or zero sperm count. At this point, advanced diagnostic or retrieval techniques might offer more clarity on the matter. Indeed, this helps specialists determine whether sperm production exists internally and assists to establish whether an assisted reproductive technique could be applicable.
All sperm qualities matter; these parameters include motility and malfunctions. Poor movement greatly reduces the chance of natural conception when sperm are present. If motility remains very low on multiple occasions, it may indicate more serious testicular or ductal deficiencies that are not able to be corrected by routine testing.
Sperm motility poor motility puts on a question of whether it is worthwhile waiting to see if anything improves with the sperm by continued testing. In cases like these, directly retrieving sperm from the source and utilizing assisted reproductive techniques may be more successful and beneficial towards saving time, especially in couples in whom age-related fertility issues may exist.
Stated another way, evaluation for male fertility may not be evident through ejaculation tests. Sometimes sperm are produced, but cannot pass through the reproductive tract due to blockages or developmental problems. This is where direct assessment becomes clinically meaningful.
The organ which is responsible for producing sperm is called testicles. Investigating them via targeted methods helps determine if sperm of appropriate quality is present. This helps physicians to take the most effective fertility pathway rather than relying on repeated external testing with limited lunations of insight.
In cases where infertility cannot be sufficiently defined by routine evaluations, physicians may suggest that minimally invasive diagnostic procedures be employed. Such procedures will help to prove sperm production internally and to better guide any further treatment planning. Particularly this is true for cases of azoospermia or of abnormal reports lasting for long periods.
The test is known as TESA treatment. It is a procedure whereby sperm is extracted directly from testicular tissue using a fine needle and does indeed provide direct evidence of sperm availability and quality so that the doctor may make a decision about whether to use assisted reproduction without delay.
Once internal sperm presence is confirmed, the focus shifts from diagnosis to action. Instead of repeatedly checking semen parameters, treatment can proceed with a clear plan. This approach reduces uncertainty and gives couples a realistic understanding of their options.
TESA treatment is often chosen when medical therapy and repeated testing fail to improve outcomes. It allows sperm retrieval even in severe male-factor cases and enables the use of advanced reproductive techniques, offering hope where conventional methods fall short.
Couples who wish to undergo assisted fertility procedures should ensure that all timing and accuracy are a must. If there is no appreciable quantity of sperm in a given semen sample, collection should be performed directly to avoid unnecessary cancellation or delay of the treatment cycle. TESA IVF is a combination of sperm retrieval and in-vitro fertilization, ensuring that fertilization occurs under controlled conditions. This is particularly useful in cases of obstructive or nonobstructive azoospermia, where sperm are produced but cannot be ejaculated.
The TESA IVF success rates look bright, provided that the procedure is appropriately indicated and performed at centers with high expertise in the procedure. One may choose to skip all the above diagnostic tests in favor of one final solution and hence shorten the fertility journey. With this, they can also get clearer and more actionable results.
Choosing Dr. Aravind's IVF means choosing professionalism, transparency, and empathetic fertility care. Thus, sperm retrieval, i.e., TESA, will boost the odds considerably for many couples; its success depends on age of female, quality of embryos, and lab competence. The center's years of expertise with complicated male and female infertility problems add a personal touch to the evidence-based care given to its patients, instead of asking them to do unnecessary repeat tests. Such advanced facilities for IVF, ICSI, and TESA ensure precise diagnoses and effective treatments under one roof.