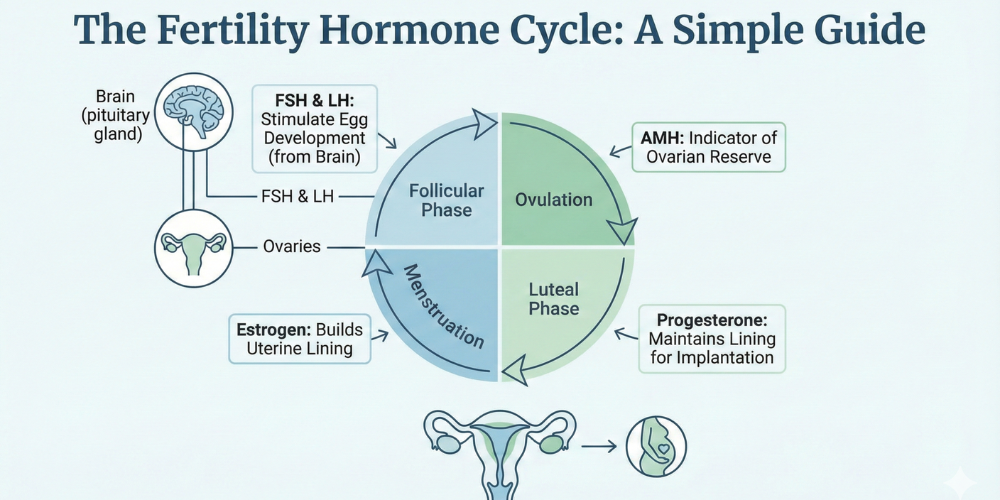
These hormones regulate female reproductive health through their complex interplay, with birth control combined with sterilization being some of the representational aspects. These hormones govern all aspects of egg development through uterine conditioning, and they are crucial to conception. By understanding the biological processes involved, women can make better, informed decisions about the fertility planning, diagnosis, and treatment services available to them. Below is a detailed explanation of some of the major reproductive processes and hormones involved in the female cycle.
It is biological ovulation, for a mature egg to leave the ovary and release itself to fertilisation. This event occurs typically once during a menstrual cycle, and will create the fertile window for conception. The timing is determined by an egg sending hormonal signals from the brain to the ovaries. Once it has been released, the egg will travel down into the fallopian tube, where it may meet a sperm. If fertilisation does not take place, the egg will dissolve away on its own, and keep the cycle in motion toward menstruation. Any disruption in this cycle, hence, would mean an impact on the fertility; hence the need for accurate cycle tracking and medical evaluation for women trying to conceive.
The Estrogen Hormone performs a major function in the female reproductive system to search and prepare the body for pregnancy. It helps in developing the ovarian follicles and thickens the lining of the uterus, facilitating implantation. This hormone exerts influence over secondary sexual characteristics and also has specific functions in bone health and cardiovascular operation. Balanced levels are critical to regular cycles: too much or too little will produce irregularities in periods, mood changes, or fertility problems. Evaluation of the hormone balance is always a component of reproductive health assessment, especially when the menstrual cycle changes.
Female hormones are coordinated by coupling all reproductive systems functions, their harmonization determining the feature of their functions: establishing menstrual cycle regulation, fertility, and reproductive aging. Their paces of release act like carefully timed chemical messengers that synchronize egg maturation, endometrial changes, and lengths of the cycle. When they alter that balance because of stress, medical problems, or age, symptoms include delayed cycles, heavy bleeding, or inability to get pregnant, but that is just one part of it. Hormonal harmony affects emotional stability, healthy skin, and levels of energy. Medically, efforts are centered on restoring that balance, either by lifestyle change or treatment, to achieve reproductive goals.
The fsh test is most useful to assess ovarian and fertility conditions. The hormone stimulates the ovaries to make mature eggs, so it is always the measurement of fsh levels in blood, the higher the quantity more indicative it would show poor ovarian reserve, whereas lower amounts indicate hormonal suppression. This test is often recommended to ladies who experience delayed periods or are unable to conceive. The results indicate the doctor on appropriate fertility treatments to opt for and how the ovaries may respond to hormonal signals from the brain.
The functions of estrogen include stimulating the endometrial lining and promoting egg maturation in the ovary. It also helps regulate cervical mucus, making it easier for sperm to travel during fertile periods. Beyond reproduction, this hormone contributes to maintaining skin elasticity, bone density, and cognitive health. Proper levels are essential for both fertility and long-term wellness. When imbalances occur, women may experience cycle irregularities or reduced chances of implantation, highlighting the importance of hormonal evaluation.
After the release of the egg, Progesterone function its main roles - it consolidates and prepares the uterine lining for the event of possible implantation. This hormone ensures stable conditions for early pregnancy, also prevents the premature shedding of the uterine lining. If there are insufficient levels of the hormone, implantation may fail or early pregnancy loss occurs. As they are especially important in fertility treatment - where at times supplementation is indicated with the aim to boost conception and maintain it - this is true.
There is relevance in knowing fsh normal range and for lh normal range in assessing fertility and menstrual health. In fact, these ranges differ in terms of age and phase during the cycle, giving insight into how well ovaries are responding to additional hormonal signals. Abnormalities indicate ovulatory disorders or hormonal imbalances that affect conception. A medical professional's accurate interpretation allows confident guiding diagnosis and treatment planning for reproductive care.
These hormonal health changes are central on female fertility as well as on reproductive wellness overall. It is with understanding what these processes would empower an individual woman to perceive imbalance signs and eventually become more inclined towards seeking proper medical advice. Evaluation and care could manage most hormonal conditions so that they may not hinder natural conception or processing by assisted reproductive means.
Fertility care provider is one of the most important decisions you can make before embarking on your parental journey; our center strives to provide both the humane fertility care tailored to the specific needs of each patient, ethical, and evidence-based. We pride ourselves upon our strong emphasis on transparency and trust in individualized attention to all clients and couples during their journeys with us.
We have well-trained specialists, cutting-edge diagnostic facilities, and progressive, clinically proven reproductive technologies that comply with international standards. We have followed a summit approach, beforehand, through an initial consultation to advanced fertility procedures. Our approach prioritizes safety, accuracy, and emotional well-being.
We believe in clear communication, honest medical guidance, and customized treatment plans rather than one-size-fits-all solutions. Consistent and safe fertility care production is possible through the combined enabling environment and continuous advancement in medicine. Establishing friendly environments with clinical expertise is a way to make parenthood accessible to every family hoping for it-informative, comfortable, and hopeful.